From Scarring to Scarless Healing: Advances in Placental Stem Cell Research
The journey of the human body begins in infancy, often characterized by seemingly flawless skin. However, as we age, the passage of time becomes visible, particularly through various types of wounds, from minor insect bites to significant surgical incisions or burns. While some wounds heal without leaving a trace, others result in persistent, often unsightly scars.
Fibrotic scars, which typically form during the healing process in adults, differ significantly from normal skin. These scars lack skin appendages such as hair follicles, sebaceous glands, and sweat glands, and are marked by a dense extracellular matrix with parallel fibers. Despite extensive research, achieving completely scarless wound healing remains a challenging goal.
Individuals dealing with scars often turn to scar removal products, but these solutions frequently yield limited results. Is there a viable approach to promote wound healing without resulting in scar tissue?
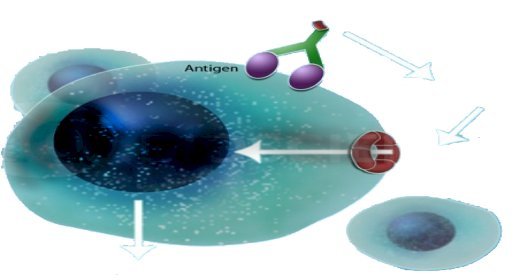
Recent advancements in modern medicine have led researchers to explore innovative solutions that leverage the body's natural regenerative abilities. One promising development involves the use of exosomes derived from placental stem cells, which offer new hope for achieving scarless wound healing.
A recent study titled "Placental Stem Cells-Derived Exosomes Stimulate Cutaneous Wound Regeneration via Engrailed-1 Inhibition," published in Frontiers, highlights the potential of these exosomes. Scar formation is closely linked to the activity of Engrailed-1 (EN1) in fibroblasts. By inhibiting EN1, researchers have found that wound regeneration can be promoted, facilitating the restoration of skin appendages and microstructures. This study also explored the benefits of mesenchymal stem cell (MSC) transplantation in reducing scar formation.
The findings revealed that placental-derived MSCs significantly accelerate wound healing. These stem cells not only hasten wound closure but also improve the quality of healing. This includes the regeneration of skin appendages like hair follicles and sebaceous glands, a decrease in collagen I levels coupled with an increase in collagen III, and improved collagen patterning within the healing skin. Additionally, MSC treatment promoted angiogenesis, highlighting the substantial potential of placental MSC-derived exosomes for wound regeneration.
Exosomes have shown capabilities beyond initial expectations. They not only inhibit scar tissue formation but also have potential applications in diagnostics and therapeutics. Exosomes can serve as diagnostic and prognostic markers, with their collection from blood, urine, and saliva offering minimally invasive diagnostic options that reduce patient discomfort.
As research advances, it is essential to consider ethical and regulatory aspects related to exosome-based therapies. Exosomes, functioning as natural carriers of signaling molecules, offer advantages such as biocompatibility, circulatory stability, and the ability to cross biological barriers. This positions them as promising candidates for developing nanocarriers and cell-mediated drug delivery systems. Furthermore, exosome-based formulations have shown efficacy in treating conditions ranging from cancer and infectious diseases to cardiovascular and neurodegenerative disorders.
In summary, the exploration of placental stem cell-derived exosomes has provided significant insights into achieving scarless wound healing. These small vesicles not only enhance skin regeneration but also hold the potential to transform diagnostics and therapeutics across various medical fields.
What's Your Reaction?















