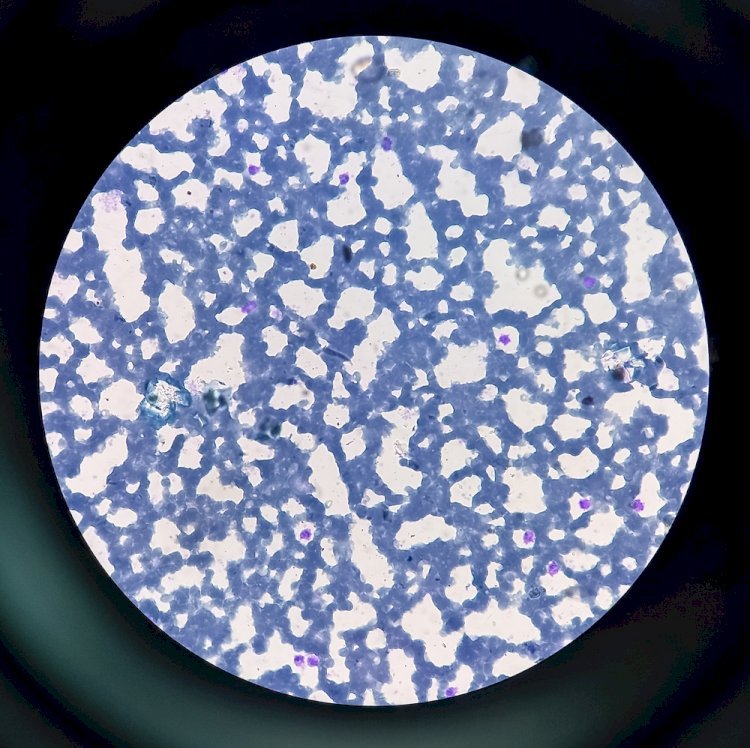
How Is Normocytic Anemia Diagnosed?
When we think about high blood pressure or hypertension, it is usually linked to lifestyle factors such as diet, physical activity, stress, or genetic predispositions. However, emerging research suggests that certain infections can also contribute to elevated blood pressure. This connection is particularly significant for those managing other health conditions like anemia, as well as patients seeking quick and convenient medical care in health facilities. Understanding this complex relationship can help in the early diagnosis of normocytic anemia, for most if not all cases.
How Infections May Lead to High Blood Pressure
Infections can impact blood pressure through various mechanisms, often involving the immune response. When the body detects an infection, the immune system releases inflammatory cytokines and other chemicals that work to fight off the invading pathogen. While this response is critical to protect the body, it can also lead to a cascade of events affecting the cardiovascular system.
-
Inflammation and Vascular Resistance
During an infection, inflammation may increase vascular resistance, or the force that the heart must overcome to pump blood through the body. This is often linked to the production of inflammatory markers such as C-reactive protein (CRP) and interleukins, which can lead to the stiffening of blood vessels. Over time, this can raise blood pressure levels.
-
Endothelial Dysfunction
Certain infections can directly affect the endothelium, the thin layer of cells that lines blood vessels. For example, bacterial infections may release endotoxins that damage these cells, reducing their ability to regulate blood vessel dilation and constriction. This imbalance may cause sustained increases in blood pressure.
-
Stress on the Cardiovascular System
Systemic infections, like sepsis or severe cases of the flu, can place significant stress on the heart. Fever, dehydration, and the metabolic demands of fighting an infection may temporarily raise blood pressure. For patients who already have risk factors for hypertension, this can push them into dangerous territory.
Infections Known to Influence Blood Pressure
Several types of infections have been studied for their potential impact on blood pressure:
-
Urinary Tract Infections (UTIs)
UTIs can lead to temporary increases in blood pressure, especially if the infection spreads to the kidneys. The kidneys play a crucial role in regulating blood pressure, and any disruption to their function can cause imbalances.
-
Respiratory Infections
Severe respiratory infections, including pneumonia and COVID-19, have been associated with elevated blood pressure in some cases. This may be due to the widespread inflammation these illnesses trigger, as well as stress on the cardiovascular system.
-
Chronic Infections
Chronic infections, like periodontal disease or Helicobacter pylori (H. pylori) infection in the stomach, can contribute to systemic inflammation, which has been linked to long-term increases in blood pressure.
The Role of Anemia and Infections in High Blood Pressure
For individuals with normocytic anemia, infections can exacerbate existing symptoms and contribute to blood pressure abnormalities. Normocytic anemia is often caused by chronic diseases or inflammatory conditions, which are themselves risk factors for both infection and hypertension. For example, patients with autoimmune conditions such as lupus or rheumatoid arthritis may have underlying inflammation that simultaneously leads to anemia and affects blood pressure regulation.
When an infection occurs in a person with normocytic anemia, the body’s already compromised ability to transport oxygen can become even more strained. This can lead to increased cardiac output as the heart works harder to compensate, potentially causing a rise in blood pressure. A visit to a Primary Care Walk-In Clinic in Texas can help individuals identify these overlapping issues and receive timely treatment, including blood tests to evaluate anemia and infection markers.
The Connection Between Chronic Inflammation and Hypertension
Chronic infections and inflammatory conditions create an environment where blood pressure can remain persistently elevated. For example, patients with infections like tuberculosis or viral hepatitis often have ongoing inflammatory responses that may affect the cardiovascular system. These responses can lead to:
- Increased oxidative stress in blood vessels
- Impaired kidney function
- Altered hormone regulation, particularly involving the renin-angiotensin-aldosterone system (RAAS), which is critical for blood pressure control
For patients managing chronic conditions alongside infections, it is essential to regularly monitor blood pressure and seek care promptly when abnormalities are detected.
Diagnosis and Management at Primary Care Clinics
The first step in addressing infection-related high blood pressure is a comprehensive diagnosis. Primary Care Walk-In Clinics in Texas are well equipped to handle a variety of health concerns, offering quick access to diagnostic tests such as blood work, urinalysis, and imaging. These clinics often serve as a one-stop solution for patients experiencing overlapping symptoms, such as fatigue from anemia, fever from an infection, and elevated blood pressure.
-
Blood Tests
Tests can measure inflammatory markers like CRP, white blood cell count, and hemoglobin levels to identify infections and anemia. For patients with normocytic anemia, these tests can help determine whether the condition is caused by an infection, chronic inflammation, or another underlying issue.
-
Blood Pressure Monitoring
Many clinics provide immediate blood pressure monitoring and follow-up care. This is especially important for identifying whether high blood pressure is temporary (due to an acute infection) or persistent, requiring longer-term management.
-
Treatment Options
Treatment at a primary care clinic may include antibiotics or antiviral medications for infections, iron or vitamin supplementation for anemia, and antihypertensive medications if necessary. Lifestyle advice, such as maintaining hydration and reducing sodium intake, may also be offered to help manage blood pressure during recovery.
When to Seek Medical Attention
While minor infections may not significantly impact blood pressure in healthy individuals, certain symptoms should prompt immediate medical attention:
- Persistently high blood pressure despite treatment for the infection
- Symptoms of severe infection, such as fever, chills, or confusion
- Signs of anemia, including fatigue, shortness of breath, and pale skin
- Swelling in the legs or difficulty breathing, which may indicate cardiovascular strain
For such concerns, a Primary Care Walk-In Clinic in Texas provides an accessible option for prompt evaluation and care. These clinics are particularly beneficial for patients who need same-day appointments but do not require the resources of an emergency room.
Preventing Complications
To minimize the risk of infection-related high blood pressure, it’s important to take preventive measures:
-
Vaccinations
Staying up-to-date on vaccinations can reduce the risk of serious infections like pneumonia and the flu, which may lead to blood pressure complications.
-
Managing Chronic Conditions
Conditions like diabetes, chronic kidney disease, and autoimmune disorders should be well-managed to reduce susceptibility to infections and associated blood pressure changes.
-
Healthy Lifestyle Choices
Regular exercise, a balanced diet, and adequate hydration can support both immune function and cardiovascular health, reducing the likelihood of complications from infections.
Conclusion
The connection between infections and high blood pressure is a reminder of how interconnected our body systems are. Whether it’s inflammation from a bacterial infection or the strain of managing a chronic illness like normocytic anemia, the effects can extend to blood pressure regulation and overall cardiovascular health. A Primary Care Walk-In Clinic in Texas is a valuable resource for addressing these complex issues and providing timely diagnosis, treatment, and follow-up care.
By staying vigilant about symptoms, seeking early medical attention, and adopting preventive measures, patients can reduce their risk of complications and maintain better overall health. Whether managing an infection, anemia, or high blood pressure, holistic care can make a significant difference in long-term outcomes.
What's Your Reaction?















