Injecting mRNA and Generating CAR-T Directly in the Body to Repair the Heart in One Shot
January 6, 2022—Researchers at the Perelman School of Medicine at the University of Pennsylvania published a research paper in Science titled: CAR-T cells produced in vivo to treat cardiac injury.
Heart damage or inflammation can induce fibroblasts to overproduce fibrous material, causing cardiac fibrosis, which hardens the heart muscle and impairs heart function. Heart failure, liver disease, and kidney failure are just a few of the major conditions that can result from cardiac fibrosis.
The FDA approved CAR-T cell therapy, also known as chimeric antigen receptor T-cell therapy, as the first CAR-T cell therapy to be marketed for the treatment of leukemia in 2017, ushering in a new age of CAR-T cell therapy.
To date, CAR-T cell therapies have necessitated the collection of a patient's own T cells, which are then genetically reprogrammed in the laboratory to recognize specific cancer cells, allowing them to identify and destroy cancer cells once they are reintroduced into the body. The entire procedure is complicated and time-consuming, resulting in a high price tag of hundreds of thousands of dollars.
The CAR-T cell therapies now on the market are all intended to treat blood malignancies, but they have shown promise in a variety of other disorders as well. Jonathan Epstein's team at the University of Pennsylvania's Perelman School of Medicine demonstrated in 2019 that CAR-T cell therapies can target overactive cardiac fibroblasts and restore heart function.
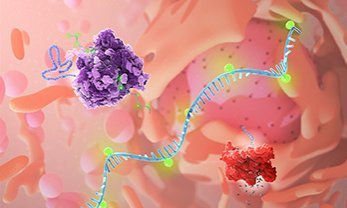
In a mouse model of heart failure, the scientists devised a transiently designed CAR-T cell therapy that reprograms T cells to detect cardiac fibrotic cells by injecting mRNA supplied by lipid nanoparticles (LNPs), which lowers fibrosis and restores cardiac function. The technology is comparable to an mRNA vaccine in that it only takes one injection to manufacture CAR-T cell therapies in vivo, and it is predicted to tackle the present issues of CAR-T treatments' complex procedure, long cycle time, and expensive price.
The paper's authors include Jonathan Epstein, chief scientist at the Perelman School of Medicine at the University of Pennsylvania, Drew Weissman, one of the founders of mRNA technology, as well as Carl June, the father of CAR-T.
The researchers created a new CAR-T cell therapy based on mRNA technology that targets fibroblast-activating protein (FAP) via mRNA recoding of the T cell receptor for distribution utilizing lipid nanoparticles (LNPs), a vector that has been widely utilized and proven in the COVID-19 mRNA vaccine. And because this LNP vector recognizes CD5, which is abundantly expressed by T cells, it can target T cells precisely and generate FAP-CAR-T cells.
The team then performed therapeutic experiments in a mouse model of heart injury, where mRNA was encapsulated by CD5/LNP and then injected into the mice. These mRNA molecules successfully entered the mouse T cells, effectively reprogramming the T cells and targeting them to attack activated fibroblasts. Because the mRNA was not integrated into the T cell genome, the reprogramming was only transitory, and the T cells recovered after a few days and no longer targeted fibroblasts. Importantly, mRNA-induced reprogramming of a high number of CAR-T cells led to a considerable decrease in cardiac fibrosis and restoration of normal heart size and function in mice in just a few days.
Because mRNA is only stable in the body for a short time (about a week), this in vivo-generated engineered CAR-T cell therapy is transient and does not act as long as traditional viral vector-based in vitro reprogrammed CAR-T cell therapies, and thus does not suppress fibroblasts for long periods of time or impair functions like wound healing.
The researchers said they'll keep testing this transitory mRNA-based CAR-T cell therapy and expect to move forward to human clinical trials as soon as possible.
What's Your Reaction?