Managing Hypertension and CKD: A Delicate Balance
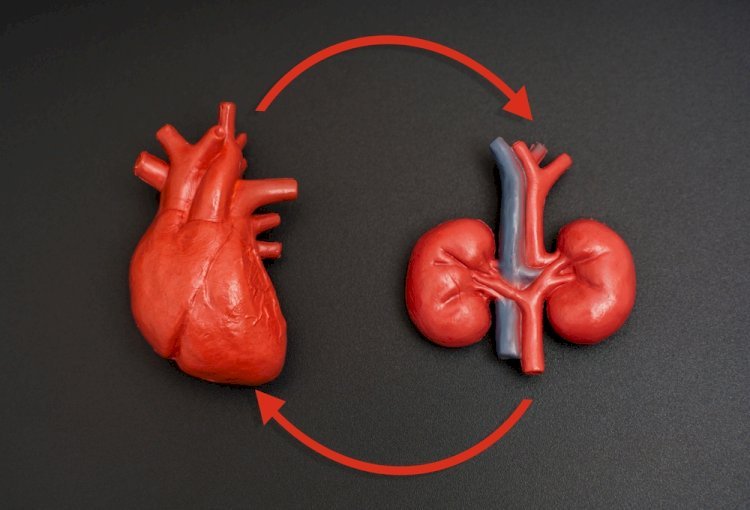
Picture this: Your body is a beautifully intricate machine, running 24/7, powered by your heart and kidneys. But what happens when these two vital organs—your heart and kidneys—start facing challenges together?
Managing Hypertension and CKD (chronic kidney disease) might sound like juggling flaming swords, but don’t worry, we’ve got the safety net ready for you! Let’s dive into this critical yet manageable health concern with some facts, precautions, and life-altering insights.
The Dynamic Duo: Hypertension and CKD
Hypertension—commonly known as high blood pressure—affects about 1.28 billion adults globally, with nearly half unaware of their condition. Chronic kidney disease (CKD), on the other hand, impacts around 10% of the population worldwide. When combined, these two conditions form a vicious cycle: hypertension damages the kidneys, and as kidney function declines, blood pressure surges further.
Fun Fact: Your kidneys filter approximately 50 gallons of blood daily, a task they can’t perform efficiently when affected by CKD. Overworking these organs due to uncontrolled hypertension is like running a marathon without breaks—it’s bound to lead to trouble!
Facts and Myths About Hypertension
Let’s clear the air about hypertension. Did you know that it’s often called the “silent killer”? This nickname isn’t a myth; hypertension can progress without noticeable symptoms. However, many believe that hypertension only affects older adults—this is a myth! Hypertension can creep into anyone’s life, even in their 20s, especially when risk factors like stress, obesity, or family history come into play.
Another common myth is that reducing salt intake solves everything. While it helps, maintaining healthy blood pressure requires a combination of diet, exercise, and sometimes medication.
Lifestyle Maintaining Approach: Small Changes, Big Impact
Living with Hypertension and CKD doesn't mean surrendering to a bland lifestyle. Instead, think of it as a chance to make empowering choices! Here’s a lifestyle maintaining approach:
- Food for Thought: Consider the DASH (Dietary Approaches to Stop Hypertension) diet. It’s packed with fruits, vegetables, whole grains, and low-fat dairy products, all heart-and-kidney-friendly. Reduce sodium intake to less than 2,300 mg daily, but don’t skimp on potassium-rich foods like bananas and spinach—they help counteract sodium's effects.
- Move It or Lose It: Regular physical activity, like walking for 30 minutes daily, works wonders for blood pressure and kidney health. It also reduces stress—one of the sneaky contributors to hypertension.
- Hydrate Smartly: While hydration is vital, those with CKD need to monitor their fluid intake to avoid overloading their kidneys. Consult your healthcare provider for the right balance.
- Stress Less: Stress management techniques like meditation or yoga can lower cortisol levels, benefiting both blood pressure and overall well-being.
Prevalence and the Global Challenge
According to a study, over 850 million people worldwide are living with kidney diseases, with hypertension being one of the leading causes. Meanwhile, the American Heart Association reports that nearly 45% of U.S. adults have hypertension, and more than 37 million Americans suffer from CKD. The intertwining of these conditions underscores the urgency for awareness and effective management strategies.
Why It’s Important to Stay on Top of Both
Think of hypertension and CKD as two friends who love drama. Left unchecked, their toxic relationship can lead to severe consequences such as heart attacks, strokes, or complete kidney failure. Regular screenings and blood pressure monitoring can keep them in check. Remember, catching CKD early could save you from needing dialysis or a transplant in the future.
Prevention is Better Than Cure
- Routine Check-Ups:
Make it a habit to monitor your blood pressure and kidney function, especially if you have a family history of these conditions. Early diagnosis can significantly delay CKD progression.
- Balanced Diet:
Steer clear of processed foods, which are packed with hidden sodium. Instead, savor natural, wholesome meals.
- Mind Your Weight:
Excess weight can increase blood pressure and strain your kidneys. Maintain a healthy BMI through regular exercise and mindful eating.
- Avoid Over-the-Counter NSAIDs:
Nonsteroidal anti-inflammatory drugs like ibuprofen can be harsh on your kidneys. Always consult a healthcare professional before taking medications.
Medications: The Frontline of Treatment
-
ACE Inhibitors and ARBs:
- These medications lower blood pressure and protect the kidneys from further damage.
- Common examples are lisinopril (ACE inhibitor) and Losartan (ARB).
2. Calcium Channel Blockers:
- These relax blood vessels, making it easier for the heart to pump blood.
- Common examples are amlodipine and Diltiazem.
3. Diuretics:
- Often called “water pills,” these help remove excess salt and water from the body, reducing blood pressure and preventing fluid overload in CKD.
- Example: Hydrochlorothiazide.
4. SGLT2 Inhibitors:
- Originally designed for diabetes management, these drugs have shown remarkable benefits in lowering blood pressure and slowing CKD progression.
- Example: Empagliflozin.
5. Beta Blockers:
- These reduce the heart's workload, decreasing blood pressure and providing cardiovascular protection.
- Example: Metoprolol.
Dietary Interventions: Food as Medicine
Nutrition is a cornerstone of managing Hypertension and CKD. Incorporate these dietary tips into your routine:
-
Low-Sodium Diet:
- Limit daily sodium intake to less than 2,300 mg, or lower if advised by your doctor.
- Replace salt with herbs and spices for flavor.
-
Fluid Management:
- CKD patients may need to restrict fluids to prevent overburdening the kidneys.
- Consult with a dietitian for tailored recommendations.
-
Plant-Based Diet:
- A diet rich in fruits, vegetables, and whole grains can reduce blood pressure and slow CKD progression.
-
Limit Phosphorus and Potassium (If Advised):
- Processed foods, dairy products, and certain fruits like bananas and oranges may need to be restricted for advanced CKD patients.
Potential Life-Changing Treatments for Hypertension and CKD
Recent advancements in medicine have opened doors to potential life-changing treatments. From medications like SGLT2 inhibitors, which reduce blood pressure and slow CKD progression, to innovative dialysis techniques, science is rewriting the playbook for managing these conditions.
The Power of Prevention: A Tale of Resilience
Imagine a 50-year-old patient, who discovered he had Hypertension and CKD during a routine check-up. Initially overwhelmed, he decided to take charge of his health by adopting the lifestyle-maintaining approach we just discussed. Within a year, he experienced improved kidney function, lower blood pressure, and a renewed zest for life. His story is a reminder that with determination, you can turn the tide in your favor.
The Road Ahead
Living with Hypertension and CKD is a delicate balancing act, but it doesn’t have to be a daunting one. By debunking myths about hypertension, embracing a lifestyle-maintaining approach, and following necessary precautions, you can effectively manage these conditions while maintaining a fulfilling life.
With advancements in medicine and growing awareness, the prognosis for patients is better than ever. Remember, your health journey is personal, but you’re never alone in it. Regular check-ups, a proactive mindset, and a supportive healthcare team are your best allies in this battle.
Let’s beat the silent killer and protect our kidneys—one healthy choice at a time!
What's Your Reaction?















