Treatment Planning Systems Market: Enabling Precision in Radiation Therapy
Introduction
Treatment planning systems are software platforms used to design and manage the delivery of radiation therapy for cancer patients. These systems play a critical role in determining the exact location, shape, and dose of radiation beams to destroy malignant tissues while minimizing damage to surrounding healthy organs.
Radiation therapy remains one of the primary methods for treating various types of cancer, and with the advancement of medical imaging and computing technologies, treatment planning systems have evolved into sophisticated tools that enhance clinical outcomes. The market for treatment planning systems is growing as healthcare providers increasingly prioritize precision, automation, and integration within oncology care.
As the demand for personalized, image-guided radiation therapy continues to rise, the global treatment planning systems market is experiencing rapid technological transformation and expansion across developed and emerging healthcare sectors.
Source: https://www.databridgemarketresearch.com/reports/global-treatment-planning-systems-market
The Evolution
Early forms of radiation therapy planning relied on manual measurements and 2D imaging such as X-rays to approximate treatment areas. These basic methods had limited precision and often led to collateral damage to healthy tissues.
The advent of computed tomography (CT) in the 1970s allowed for cross-sectional imaging, giving clinicians the ability to map tumors more accurately. This paved the way for three-dimensional treatment planning, improving dose distribution and patient safety. By the late 1980s and 1990s, treatment planning systems began integrating CT, MRI, and PET scans to define target volumes more precisely.
Over time, treatment planning systems incorporated inverse planning algorithms, which calculate optimal beam configurations automatically based on the desired dose to the tumor and limits on exposure to nearby organs. The introduction of intensity-modulated radiation therapy (IMRT), volumetric modulated arc therapy (VMAT), and stereotactic techniques further increased the need for complex software platforms.
In the current era, artificial intelligence and cloud-based systems are being integrated into treatment planning to optimize workflows, enable adaptive therapy, and improve efficiency in radiation oncology departments. These advances have redefined the capabilities and expectations of treatment planning systems.
Market Trends
Widespread adoption of image-guided radiation therapy techniques
Increased use of multi-modality imaging for tumor delineation
Expansion of cloud-based and web-enabled treatment planning platforms
Integration of artificial intelligence for plan optimization
Emergence of adaptive radiotherapy for dynamic tumor tracking
Demand for personalized cancer treatment and dose escalation protocols
Development of automated contouring and segmentation tools
Growth of proton and heavy ion therapy driving specialized planning software
Global increase in cancer incidence and radiotherapy installations
Telemedicine and remote planning services in oncology
Rise in outpatient and ambulatory radiation treatment centers
Focus on dose accumulation and cumulative dose assessment tools
Integration with oncology information systems and electronic health records
Adoption of hypofractionated treatment regimens
Vendor-neutral platforms supporting diverse delivery systems
Development of mobile applications for planning visualization
Improved user interfaces for radiation oncologists and dosimetrists
Workflow automation and scripting capabilities for clinics
Higher demand for multi-user collaboration and interoperability
Standardization of DICOM and HL7 for seamless data exchange
Challenges
High cost of software licensing and system maintenance
Need for specialized training for radiation oncology teams
Complexity in integrating with legacy linear accelerators
Lengthy commissioning and validation requirements
Data privacy and cybersecurity concerns in cloud-based solutions
Limited access in low-resource and rural healthcare settings
Delays in treatment due to plan generation or revision cycles
Compatibility issues with imaging and delivery equipment
Steep learning curve for new advanced planning platforms
Interoperability limitations between vendor systems
Risk of errors during automated contouring or plan approval
Regulatory requirements and clinical validation hurdles
High capital investment needed for multi-modality planning
Resistance from staff to transition from older planning systems
Shortage of skilled dosimetrists and medical physicists
Variation in reimbursement policies for radiation procedures
Technical challenges in adaptive and real-time planning
Inconsistent implementation of AI and machine learning tools
Integration complexity with hospital-wide IT infrastructure
Ongoing need for frequent software updates and patching
Market Scope
By Modality
Photon Therapy Planning
Proton Therapy Planning
Brachytherapy Planning
Stereotactic Radiosurgery (SRS) Planning
Stereotactic Body Radiation Therapy (SBRT) Planning
Adaptive Therapy Planning
By Technology
2D Treatment Planning
3D Conformal Planning
IMRT and VMAT Planning
Image-Guided Radiation Therapy (IGRT) Planning
Motion Management and Gated Therapy Planning
Artificial Intelligence-Based Planning
By Component
Software
Services
Support and Maintenance
By Application
Oncology
Neurosurgery
Palliative Care
Research and Education
By End User
Hospitals
Radiation Therapy Centers
Academic and Research Institutions
Cancer Specialty Clinics
By Deployment
On-Premise
Cloud-Based
Hybrid Deployment
By Region
North America
Europe
Asia-Pacific
Latin America
Middle East and Africa
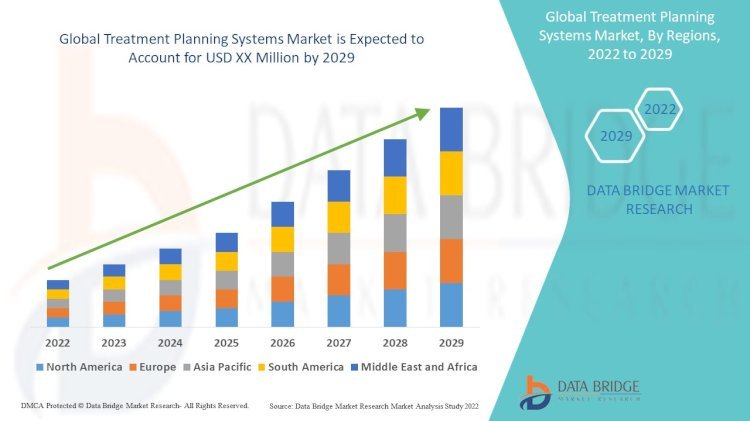
North America holds the largest share due to a well-established healthcare infrastructure and high cancer treatment rates. Europe follows with extensive adoption of radiotherapy and government support for oncology centers. Asia-Pacific is witnessing robust growth due to expanding healthcare access, rising cancer prevalence, and increasing investments in modern radiotherapy. Latin America and the Middle East are gradually adopting treatment planning systems through public-private partnerships and medical tourism.
Market Size
The global treatment planning systems market was valued at USD 1.6 billion in 2024 and is expected to reach USD 3.4 billion by 2030, growing at a compound annual growth rate (CAGR) of 12.5% during the forecast period.
The software segment dominates the market due to continuous development in planning algorithms, user interface design, and advanced modules for adaptive and proton therapy. The services segment is also expanding, as more clinics seek support in implementation, training, and cloud integration.
Oncology applications account for the majority of market revenue, as treatment planning is a foundational component of radiation therapy for cancers like lung, breast, prostate, brain, and colorectal. The growing use of stereotactic techniques and hypofractionated regimens is further fueling demand for accurate and real-time planning solutions.
Factors Driving Growth
Rising global cancer burden and need for radiation treatment
Advances in imaging technology enhancing treatment precision
Surge in proton therapy and particle-based treatments
Adoption of personalized medicine in oncology care
Growing number of radiation therapy centers worldwide
Technological advancements in contouring and plan automation
Increasing investment in oncology software infrastructure
Integration of AI for plan verification and dose optimization
Rise in hybrid radiotherapy models and remote planning capabilities
Government funding and public health initiatives for cancer care
Expansion of radiotherapy to rural and underserved areas
Higher awareness among healthcare professionals about treatment quality
Automation reducing planning time and increasing throughput
Growing number of oncology specialists requiring modern planning tools
Improved accuracy reducing complications and enhancing patient safety
Development of advanced scripting and plugin customization
Shift toward cloud-hosted solutions for scalability and collaboration
Regulatory focus on radiation safety and standardized protocols
Partnerships between software developers and academic institutions
Availability of modular and upgradeable software systems
Conclusion
The treatment planning systems market is a cornerstone of modern radiation oncology. As healthcare systems strive to deliver precise, effective, and safe cancer treatment, these systems enable clinicians to plan and manage therapy with accuracy and confidence.
With technological innovation, increasing demand for radiotherapy, and a focus on personalized care, the market continues to evolve rapidly. Challenges such as high costs, integration complexity, and training requirements remain, but ongoing innovation and collaboration across the healthcare ecosystem are helping to overcome these hurdles.
The future of treatment planning lies in AI-enabled automation, real-time adaptive planning, and cloud-based collaboration, empowering clinicians to deliver better outcomes for cancer patients globally.
What's Your Reaction?